Recently updated on December 6th, 2024 at 05:28 am
Vascular dementia, often considered the second most common type of dementia after Alzheimer’s disease, arises from problems in the supply of blood to the brain. At its core, the brain is like any other organ: it needs a steady stream of oxygen and nutrients to function effectively. When this supply is interrupted or reduced, brain cells can be damaged or die, leading to the symptoms of vascular dementia. Think of it like a thriving city. If roads and highways (our blood vessels) are blocked, parts of the city (our brain) can’t function optimally.

Understanding the connection between vascular health and cognitive decline
The health of our blood vessels plays a pivotal role in maintaining cognitive abilities. Chronic conditions such as hypertension, diabetes, and high cholesterol can damage vessels over time, causing them to narrow or become blocked. When this happens, it limits blood flow to certain parts of the brain, which can manifest as cognitive impairment.
This isn’t just about memory lapses. We’re talking about a spectrum, from mild cognitive challenges to severe disruptions in daily life. Emotionally, it can be distressing to realize that one’s vascular health directly influences one’s mental sharpness. But, this knowledge also provides a glimmer of hope: by managing vascular health, there’s potential to stave off or reduce cognitive decline.
Differentiating vascular dementia from other types of dementia like Alzheimer’s
While both vascular dementia and Alzheimer’s disease can have overlapping symptoms, their causes and progression differ significantly. Alzheimer’s is characterized by the accumulation of abnormal protein structures in the brain, known as plaques and tangles. These disrupt communication between brain cells, leading to their eventual death.
Vascular dementia, on the other hand, is caused by reduced blood flow to the brain. Its symptoms might appear suddenly after a stroke, or they might develop gradually because of a series of minor strokes or other conditions affecting small blood vessels. It’s also worth noting that while memory loss is often the primary symptom of Alzheimer’s, the first symptom of vascular dementia is often problems with thinking or reasoning.

Causes, Risk Factors, and Diagnosis of Vascular Dementia
Relationship between vascular dementia and cerebrovascular diseases
Cerebrovascular diseases are disorders that affect blood vessels and blood circulation in the brain. A direct link exists between such diseases and vascular dementia. When blood vessels are damaged or blocked, parts of the brain can become deprived of oxygen and nutrients. Over time, this can lead to the brain cell damage responsible for the cognitive impairments seen in vascular dementia. Strokes, or “brain attacks,” are one of the primary cerebrovascular events associated with vascular dementia, but other minor or silent events can also contribute.
Exploring vascular risk factors (e.g., high blood pressure, diabetes, smoking)
Several vascular risk factors can increase the likelihood of developing vascular dementia.
- High Blood Pressure: Prolonged hypertension can lead to damage of the arterial walls and small blood vessels in the brain.
- Diabetes: Poor blood sugar control can damage blood vessels, including those leading to the brain.
- Smoking: Tobacco smoke narrows and damages blood vessels, reducing blood flow to the brain.
Addressing these risk factors can go a long way in preventing or delaying the onset of vascular dementia.
Impact of cardiovascular health on the development of vascular dementia
The heart and the brain share an intimate connection. A healthy heart effectively pumps blood, ensuring a steady supply to vital organs, including the brain. When cardiovascular health deteriorates due to conditions like heart disease or atrial fibrillation, the risk for reduced blood flow or clots that block blood vessels in the brain increases. Over time, this can lead to the brain damage characteristic of vascular dementia. Hence, maintaining cardiovascular health is not just about the heart; it’s about the mind too.
Diagnostic criteria and assessment tools for identifying vascular dementia
Diagnosing vascular dementia can be complex, given its overlap with other types of dementia. Clinicians generally rely on:
- Medical history: Understanding previous cerebrovascular events, risk factors, and symptom onset.
- Neuropsychological tests: Assessing memory, attention, and problem-solving abilities.
- Clinical criteria: The National Institute of Neurological Disorders and Stroke and the Association Internationale pour la Recherche et l’Enseignement en Neurosciences (NINDS-AIREN) criteria are often used.
Role of neuroimaging techniques in diagnosing and monitoring vascular dementia
Neuroimaging has revolutionized our understanding and diagnosis of dementia. For vascular dementia, techniques such as MRI and CT scans are invaluable. They can visualize the extent of brain damage, strokes, or other vascular problems in the brain. These images can not only aid in diagnosis but also help monitor the progression of the disease or the effectiveness of interventions.

Understanding the Symptoms and Stages of Vascular Dementia
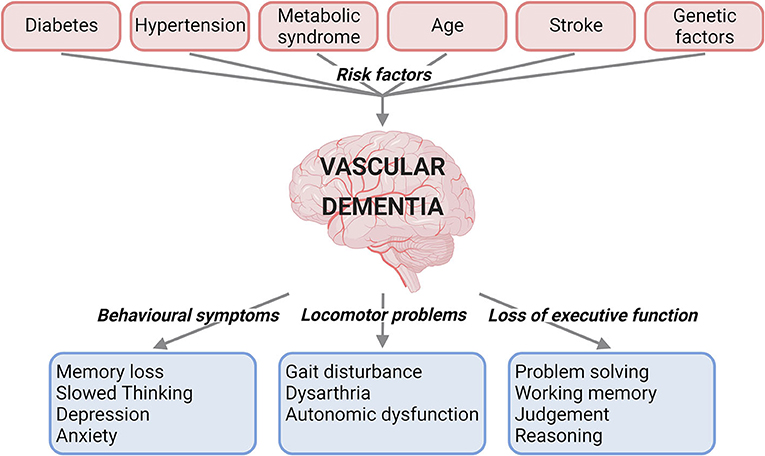
Cognitive impairment and memory loss in vascular dementia
Unlike Alzheimer’s, where memory loss is often the initial symptom, vascular dementia might present first with cognitive impairments. These can encompass difficulty with problem-solving, planning, attention, or reasoning. Memory can be affected, especially in later stages, but it’s not always the primary challenge. Individuals may struggle with processing speed, making it challenging to keep up with conversations or execute tasks promptly.
Behavioral and psychological symptoms associated with vascular dementia (BPSD)
Behavioral and psychological symptoms of dementia (BPSD) can be distressing for both the individual and their caregivers. In vascular dementia, these might include:
- Depression: A pervasive sense of sadness, loss of interest in previously enjoyed activities, or feelings of hopelessness.
- Apathy: Lack of interest or emotion, which can be mistaken for depression.
- Agitation: This can manifest as restlessness, irritability, or verbal and physical aggression.
- Hallucinations or delusions: Less common than in some other dementias, but still possible.
Understanding and recognizing these symptoms early can help in managing them effectively.
Disease progression and stages of vascular dementia
Vascular dementia’s progression can be quite variable, depending largely on the underlying causes. While Alzheimer’s tends to have a steady decline, vascular dementia might show a stepwise progression, with periods of stability followed by rapid declines. This can often be linked to cerebrovascular events like strokes.
Broadly, the stages can be categorized as:
- Early stage: Mild cognitive impairments, challenges in problem-solving or planning.
- Middle stage: More noticeable symptoms, including memory loss, confusion, and difficulty in daily activities.
- Late stage: Severe cognitive decline, where one might require assistance with most tasks and might lose the ability to communicate or recognize loved ones.

Identifying and managing sundowning in individuals with vascular dementia
Sundowning refers to an increase in confusion, agitation, and other behavioral symptoms during the late afternoon and evening. While it’s more commonly associated with Alzheimer’s, it can occur in vascular dementia too. It’s theorized to be linked to disruptions in the internal body clock, lighting changes, or fatigue.
Managing sundowning often requires a multi-faceted approach:
- Maintain routine: Keeping a consistent daily routine can help minimize confusion.
- Limit naps: Especially in the late afternoon, to ensure better sleep at night.
- Increase light exposure: Natural light during the day and ensuring the living area is well-lit in the evening can help.
- Stay calm and reassuring: If agitation arises, a calm and soothing approach is often beneficial.
Treatment and Management of Vascular Dementia
Pharmacological interventions for vascular dementia
There isn’t a cure for vascular dementia, but there are medications that can help manage some of its symptoms:
- Anti-dementia drugs: While primarily developed for Alzheimer’s, drugs like Donepezil or Galantamine can help improve cognition in some people with vascular dementia.
- Antidepressants: For those exhibiting depressive symptoms, selective serotonin reuptake inhibitors (SSRIs) might be prescribed.
- Blood-thinning medications: Aspirin or other anticoagulants can help reduce the risk of further strokes in those with certain types of vascular dementia.
- Medications for hypertension and cholesterol: Controlling blood pressure and cholesterol levels is crucial to prevent further damage.
Non-pharmacological interventions to promote cognitive stimulation and physical exercise
Engaging in regular cognitive and physical activities can be instrumental in managing vascular dementia:
- Cognitive Stimulation: Activities like puzzles, reading, or memory games can help keep the brain engaged.
- Physical Exercise: Regular physical activity like walking, tai chi, or gentle aerobics can boost brain health and improve mood.
- Occupational Therapy: Tailored interventions can help individuals maintain independence for longer.
Caregiving and support strategies for individuals with vascular dementia
Caregiving for someone with vascular dementia requires patience, understanding, and a range of adaptive strategies:
- Establish routine: A predictable routine can reduce confusion and agitation.
- Safe Environment: Ensure a fall-proof environment, use labels or color codes for better recognition.
- Effective Communication: Speak clearly, maintain eye contact, and use simple sentences. Active listening is key.
- Join Support Groups: It provides a platform for caregivers to share experiences and coping mechanisms.
Addressing vascular dementia-associated psychosis and aggression
When faced with hallucinations, delusions, or aggressive behavior, it’s essential to approach with calmness and empathy:
- Avoid confrontation: Arguing with someone experiencing a delusion can escalate the situation.
- Distraction techniques: Shifting focus to another activity can sometimes ease the situation.
- Medication: Antipsychotics may be used, but they come with potential side effects and should be a last resort.
- Seek professional counselling : It can provide strategies tailored to individual challenges.
Importance of lifestyle factors (e.g., diet, exercise) in preventing and managing vascular dementia
Lifestyle plays a pivotal role:
- Diet: A heart-healthy diet, like the Mediterranean diet, rich in fruits, vegetables, whole grains, and lean protein, can benefit both heart and brain.
- Exercise: Regular physical activity keeps blood vessels healthy and enhances cognitive function.
- Avoid Smoking and Limit Alcohol: Both are risk factors for vascular problems.
- Manage Stress: Chronic stress can exacerbate vascular issues, so practicing relaxation techniques like meditation can be beneficial.
Comparison and Distinction: Vascular Dementia vs. Alzheimer’s Disease
Differentiating characteristics and symptoms of vascular dementia and Alzheimer’s
Both Alzheimer’s disease and vascular dementia are leading causes of cognitive impairment, but they have distinct origins and manifestations:
- Onset: Vascular dementia often presents suddenly after a stroke or series of mini-strokes, while Alzheimer’s typically has a more insidious, gradual onset.
- Symptom Progression: Vascular dementia might display a stepwise progression, where periods of stability are followed by rapid declines. In contrast, Alzheimer’s generally follows a steady, predictable decline.
- Primary Symptoms: Vascular dementia might first show difficulty with planning, reasoning, or problem-solving. With Alzheimer’s, memory loss is usually the primary and initial symptom.
- Brain Changes: Alzheimer’s is characterized by plaques and tangles, while vascular dementia results from reduced blood flow to the brain due to damaged blood vessels.
Overlapping risk factors and comorbid cases of vascular dementia and Alzheimer’s
There’s a significant overlap in risk factors for both conditions:
- Age: The risk of both conditions increases with age.
- Genetic Factors: Certain genes can predispose individuals to either condition.
- Cardiovascular Health: Factors such as high blood pressure, high cholesterol, and diabetes are risks for both Alzheimer’s and vascular dementia.
It’s not uncommon to find cases where both Alzheimer’s and vascular dementia co-exist, termed ‘mixed dementia.’ Here, symptoms of both conditions may be present, often making the condition more challenging to manage.
Challenges in accurately diagnosing and treating individuals with mixed dementia
Diagnosing mixed dementia can be particularly challenging due to the overlapping symptoms:
- Clinical Assessments: While neuroimaging can reveal brain changes typical of both Alzheimer’s and vascular dementia, it might be challenging to ascertain which symptoms are attributed to which condition.
- Symptom Complexity: Mixed dementia can result in a broader range of cognitive impairments than either condition alone.
- Treatment Dilemma: Treating mixed dementia requires a nuanced approach, balancing interventions for Alzheimer’s and managing vascular risk factors simultaneously.
Future Research and Perspectives on Vascular Dementia
Promising developments in the field of vascular dementia research
The landscape of vascular dementia research is ever-evolving, aiming to unlock deeper insights and improved interventions:
- Molecular Mechanisms: Advances in neurobiology have begun to elucidate the molecular and cellular mechanisms behind vascular dementia, providing avenues for potential therapeutic targets.
- Gene Therapy: Recent studies are focusing on the role of specific genes in vascular dementia, with the hope that gene therapies might eventually offer solutions.
- Stem Cell Research: The potential for stem cells to repair damaged blood vessels or even replace damaged brain tissue offers a promising frontier in vascular dementia research.
Impact of ongoing studies on early detection, prevention, and more targeted treatment options
Ongoing research promises significant impacts:
- Biomarkers: Identifying biomarkers in blood or cerebrospinal fluid could offer earlier detection long before pronounced symptoms appear.
- Prevention Studies: Trials are underway examining how interventions like blood pressure control and cholesterol-lowering might directly impact the onset or progression of vascular dementia.
- Tailored Treatments: As we gather more data, treatments can be more precisely tailored to individual patients based on their specific risk factors, genetics, and symptom profiles.
Conclusion
Summary of key points discussed
Vascular dementia, a consequence of reduced blood flow to the brain, stands distinct from other dementias like Alzheimer’s, though they share overlapping risk factors. While current treatments focus on symptom management and vascular health optimization, future research holds the promise of more targeted interventions.
Encouragement to seek medical advice and support for individuals and caregivers
For anyone suspecting they or a loved one might be facing vascular dementia, it’s paramount to seek medical advice early. Early detection and intervention can significantly influence disease progression. Moreover, support groups and community resources can provide invaluable assistance to caregivers, offering both emotional support and practical caregiving strategies.
Empowering individuals to adopt a healthy lifestyle and reduce vascular dementia risk
While the future is optimistic with ongoing research, we must not overlook the power of prevention. Adopting a heart-healthy lifestyle, engaging in regular physical activity, managing stress, and addressing vascular risk factors proactively can play a substantial role in reducing the risk of vascular dementia.
Sources
- Mayo Clinic. (2019). Vascular dementia – Symptoms and causes
- National Institute on Aging. (2017). Vascular contributions to cognitive impairment and dementia
- Alzheimer’s Association. (2020). Brain changes associated with Alzheimer’s disease
- Alzheimer’s Society. (2018). Different types of dementia explained
- Johns Hopkins Medicine. Cerebrovascular Disease
- Alzheimer’s Research UK. (2020). Vascular dementia: Causes and risk factors
- World Health Organization. (2019). Tobacco and cardiovascular disease
- American Heart Association. (2017). Brain health is linked to heart health
- Román, G.C. et al. (1993). Vascular dementia: diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop
- Dementia Care Central. (2020). How Vascular Dementia Is Diagnosed: Tests & Criteria Used
- Alzheimer’s Association. (2020). Vascular dementia signs and symptoms
- Dementia UK. (2018). Depression and dementia
- National Institute for Health and Care Excellence (NICE). (2018). Dementia: assessment, management and support
- Spector, A., Thorgrimsen, L., Woods, B., et al. (2003). Efficacy of an evidence-based cognitive stimulation therapy programme for people with dementia
- Ballard, C., & Corbett, A. (2010). Management of neuropsychiatric symptoms in people with dementia
- Harvard Health Publishing. (2018). Vascular dementia: A name for a batch of specific conditions
- National Institute on Aging. (2017). What Is Mixed Dementia?
- Alzheimer’s Society. (2019). Mixed dementia
- Horsburgh, K., Wardlaw, J. M., van Agtmael, T., Allan, S. M., & Ashford, M. L. J. (2018). Small vessels, dementia and chronic diseases – molecular mechanisms and pathophysiology. Clinical Science, 132(8), 851-868
- National Institutes of Health. (2019). Genetics and Vascular Dementia
- Bachstetter, A. D., & Pabon, M. M. (2016). The Entry of Stem Cells into the Brain for Treatment of Vascular Dementia. Current Alzheimer Research, 13(5), 538-544
- Skrobot, O. A., Attems, J., & Esiri, M. (2016). Vascular Cognitive Impairment Neuropathology Guidelines (VCING): the contribution of cerebrovascular pathology to cognitive impairment. Brain, 139(11), 2957-2969
