Recently updated on January 21st, 2026 at 10:53 am

With projections showing a 29% increase in Californians with Alzheimer’s by 2025 and a 40% rise in Los Angeles County by 2030, dementia is a growing concern, particularly affecting Latino and Asian communities, where cases are expected to double. These trends highlight the urgent need for effective care strategies.
In California, caregivers provide over 1.8 million hours of unpaid care annually, valued at $23 billion, with 59% reporting high emotional stress. The total cost of dementia care in the U.S. is estimated at $781 billion in 2025, underscoring the financial and emotional toll on families.
However, there are many ways to make the lives of those affected and those around them much easier. To do that, it’s important to know the causes, symptoms, and different methods to help.
Dementia Symptom
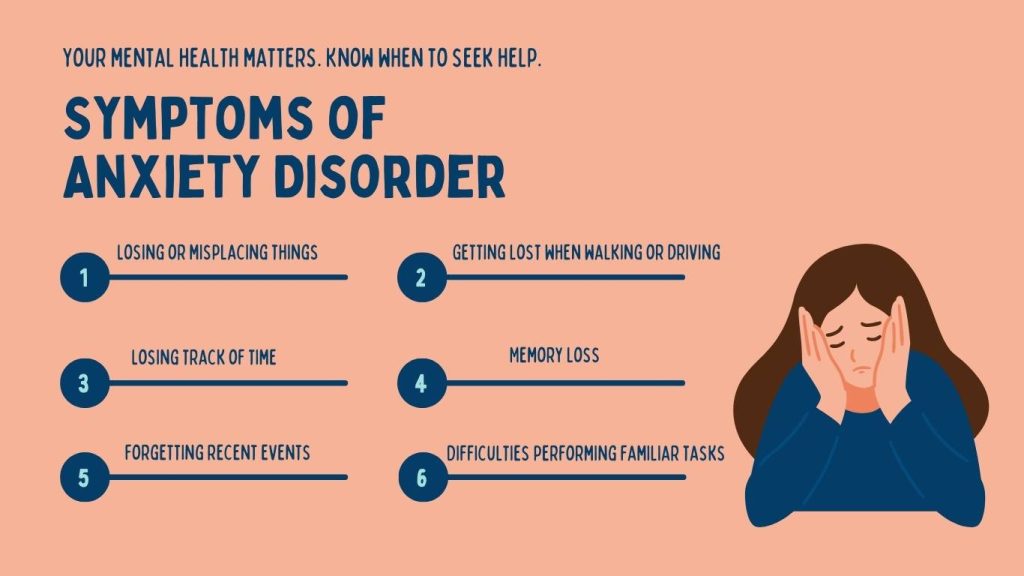
People affected by dementia lose their ability to negotiate new information and stimulus. This lack of mental functioning results in creating the following symptoms in patients.
Cognitive Changes
- Losing or misplacing things
- Getting lost when walking or driving
- Losing track of time
- Difficulties solving problems or making decisions
- Memory loss (which is usually noticed by other people)
- Problems following conversations or trouble finding words
- Difficulties performing familiar tasks
- Forgetting recent events
- Problems communicating or finding the right words
Dementia Behavioral Changes

- Feeling anxious, sad, or angry (because of memory loss)
- Personality changes
- Withdrawal from work or social activities
- Being less interested in other people’s emotions
- Depression
- Inappropriate behaviour
- Paranoia
- Hallucination
- Along with their cognitive decline, the symptoms above will contribute to causing relentlessness and Agitation in Dementia patients.
Aggression in Dementia

As dementia progresses, the person may show signs of dementia aggression. This will be distressing for people around them.
Dementia causes problems in conversing. So there are limited ways for patients to tell others what causes them agitation or distress.
Experiencing distress, agitation, and discomfort for extended periods will lead to signs of aggression in anyone.
To alleviate aggressiveness, it’s essential to see beyond the behavior and consider what may cause it.
Some everyday situations that may lead to agitation and distress include:
- Fear and fatigue (from trying to make sense of a new confusing world)
- Environmental changes, such as travel, hospitalization, or the presence of houseguests
- Their mental and physical health – for example, they may have discomfort or pain that they are unable to communicate or solve
- Moving to a new location or nursing home
- Feeling that they’re not being listened to or understood
Dementia can affect a person’s personality and habits. However, a person who has never been aggressive before may not show drastic signs of aggression, if any at all.
Dementia Aggression Treatment

Agitation and aggression happen for a reason, even if the cause is unclear to us. To combat this, you must first understand the person and the source of this aggression.
If someone starts showing signs of aggression, then try to find the causes and do your best to remove them. Below are some tips that’ll help reduce and remove aggression:
- Limit the amount of caffeine intake the person drinks
- Keep a routine, such as bathing, dressing, and eating at the same time each day
- Speak calmly to them. Listen to their concerns and frustrations
- Show them that you understand if the person is angry or fearful
- Keep well-loved objects like photographs around the house to help the person feel more secure
- Use soothing music, reading, or walks
- Reduce noise
- Try to distract them with a favourite snack, object, or activity.
If Patients Become Overly Aggressive
If the person’s aggression escalates to screaming and possibly physical harm, then protect yourself and others.
If you have to stay, then keep a distance from them. Also, try to protect the person from harming themselves.
Safe Environment for Dementia Patients
Dementia patients require constant monitoring and an environment that prevents their lack of cognitive capacity from damaging themselves.
Use locks

View people with dementia as children. Anything that may potentially harm them needs to be kept locked away. That includes anything that could possibly cause harm, such as medicines, alcohol, cleaning supplies, guns, dangerous utensils, and tools.
Adjust Water Temperature

Adjusting the water to a lower temperature will prevent people with dementia from getting burnt.
Prevent falls

Avoid leaving extension cords, scatter rugs, papers, or any type of items that may cause them to fall. You may even add plastic mats in the bathroom for extra precautions.
What is a Risk Factor? And What are Some Dementia Risk Factors?
Risk factors include the aspects of lifestyles and things that can increase the chances of developing a disease.
On their own, they can not cause a disease. Instead, they increase the chances of developing the said disease.
Aging is a primary risk factor, with dementia prevalence rising sharply in California’s aging population. By 2025, the number of Californians with Alzheimer’s is projected to increase by 29%, with significant disparities expected among Latino, Asian, and African-American communities in Los Angeles.
Avoiding dementia risk factors doesn’t guarantee a 100 percent chance of not developing the disease. But preventing and solving the following issues can drastically reduce the chances.
- Smoking
- Poor diet
- High Blood Pressure
- High alcohol consumption
- Lack of Cognitive Engagement
- Depression
- Social Isolation
Why do Physical Risk Factors Cause Dementia?
Smoking
Long-term exposure to cigarette smoke is linked to oxidative stress, which is connected to the onset of dementia.
Smoking also increases the chances of developing risk factors for Alzheimer’s disease, strokes, and hypertension.
High Blood Pressure
The risk of dementia, particularly vascular dementia, increases when someone also has high blood pressure.
People with consistently high blood pressure, mainly from 45 to 65, have a higher chance of developing dementia compared to those with normal blood pressure.
High Alcohol Consumption
Excessive alcohol consumption is one of the strongest risk factors for developing dementia. This is because immoderate drinking causes neurotoxic effects on the brain.
Poor Diet
Having heart issues can increase your chances of developing dementia. So, to reduce the chances of developing the disease, it’s essential to consume a diet suitable to upkeep your heart.
Too much saturated fat can contribute to high cholesterol levels, too much salt can result in high blood pressure (hypertension), and too much sugar raises the risk of type 2 diabetes. These conditions are also associated with poor heart health and the chances of dementia.
Why Do Psychological Risk Factors Cause Dementia?
Social Isolation
Social Isolation causes several diseases which promote dementia. Some include high blood pressure, heart disease, obesity, anxiety, depression, cognitive decline, and much more.
Depression

Depression can impair cognitive functions. People who experience this mental ailment in mid- or later life have a higher risk of developing dementia.
Whether depression is a risk factor is still unclear. Many believe this theory; others say that depression is an early sign of dementia, while some think it’s both.
Lack of Cognitive Engagement
Engagement in cognitively stimulating work and activities may slow cognitive decline and dementia.
Think of your brain as a muscle. The more you use it, the stronger and healthier it becomes. The same is said about our cognitive decline.
If a person is regularly engaged in social and cognitive activities, they will increase their cognitive ability and reduce the chances of developing dementia.
Innovative care models are emerging to address these challenges. In Los Angeles, programs like the Healthy Brain LA Coalition bring together over 90 partners to promote early detection and caregiver support, while technologies such as telehealth and remote monitoring enhance home-based care and safety.
Dementia Care for loved ones
If you’re caring for a loved one, know that your role in managing daily tasks will increase as the disease progresses.
To combat the strain of being a caretaker, try to limit the challenges. Below are some easy ways to reduce the stress from caretaking while still giving your dependant the care they need.
Schedule wisely

Tasks like bathing and Medication Management are more manageable when the person is most alert and refreshed.
Involve the person
Let them do as much as possible. This strategy will allow them to feel less sick and much more refreshed. It’ll also give you a little time for personal care. Just ensure the stuff you ask of them is easy, e.g., setting the table.
Follow the doctor’s advice
Make sure you keep a doctor in your life. Ask professionals what needs to be done and try implementing their advice. Avoid missing checkups.
Caregivers in Los Angeles and Orange County can access resources like the UCLA ADC Project ECHO, which provides evidence-based training through interactive sessions, and the GUIDE program, which offers care coordination to keep patients at home and reduce stress on families.
Intervention for Dementia Care
Being a full-time caretaker for dementia patients is a lot of work. Especially if the caregiver has another occupation, the everyday schedule of working and being a full-time caregiver can sometimes feel overwhelming.
If at any time you feel like the work is too much to handle, then don’t be afraid to ask for help. You could reach out to family members to help watch or provide you Assistance with Daily Living.
If you’re unable to rely on assistance from family, innovative programs like the CMS GUIDE model use care navigators to coordinate medical and social services, while UCLA’s ADC Project ECHO offers interactive training for caregivers and providers. These approaches help reduce hospitalizations and improve outcomes for dementia patients in Los Angeles and Orange County.
Conclusion
Dementia isn’t a life-threatening illness. But it can cause poor quality of life. Therefore, it’s essential for us and our loved ones to avoid any risk factors that may cause this disease. And use whichever means to help the loved ones that are already affected.
Though dealing with a dementia patient is challenging, it doesn’t make it impossible. Our modern society provides several ways to support our elders. The community’s professionals can help assist in caretaking duties and provide the advice needed to help dementia patients.
By having the assistance and the right amount of knowledge, you’d be able to properly care for those affected and help prevent others from developing dementia.
